Toilet Seat Pain

Slideshow: Back Pain Myths and Facts What Are Sciatica Causes? What Are Sciatica Risk Factors? What Are Symptoms of Sciatica? When Should Someone Seek Medical Care for Sciatica? What Tests Do Health-Care Professionals Use to Diagnose Sciatica? What Are Home Remedies for Sciatica? What Are Sciatica Medications and Treatments? Is Surgery Necessary for Sciatica? What Are Other Forms of Therapy for Sciatica? What Steps Can Help Prevent Sciatica? What Is the Prognosis of Sciatica? Read more on Sciatica from Healthwise The most common symptom from sciatica is pain. Most people describe a deep, severe pain that starts low on one side of the back and then shoots down the buttock and the leg with certain movements. Sciatica can also cause knee pain, hip pain, and foot pain. Catherine Burt Driver, MD William C. Shiel Jr., MD, FACP, FACR Must Read Articles Related to Sciatica An abscess is has several causes and can appear o...learn more >>

Blood is supposed to clot to help repair a blood vessel that is injured. Clots or thrombi become a problem when they form inappropriately. There are a variety o...learn more >> Chronic pain is pain that persists for a period of six months or longer, and is the result of a long-standing medical condition(s) or damage to the body. See the Entire Sciatica Topic Guide » What treatments have been helpful with your sciatica? Sciatica - Describe Your Experience Please describe your experience with sciatica. What were the symptoms of your sciatica?Raised toilet seats are divine inventions for those who have trouble bending to sit on a standard toilet seat. These elevated devices are routinely prescribed for short term use upon hospital discharge, usually to accommodate fractures or post-hip replacements and knee surgeries. Elderly individuals and those with chronic arthritis, hip pain, knee pain, back pain or mobility issues may require a more permanent solution to maintain independence in the bathroom.

Sizes, prices and safety mechanisms vary considerably so you need to know your options. Optimal Seat Height: Raised toilet seats sit atop the stool and typically add between 2 inches and 6 inches in height. The higher the seat, the less flexion is required in your hips and knees, making it easier to sit down and stand up. If your toilet seat is too high, however, you will feel unstable. The ideal height is one where your feet are flat on the floor. You can also elevate your toilet seat by raising the entire toilet from underneath. Allegro Medical sells a toilet seat riser that doesn’t change the look of your standard toilet but will raise it about 3.5″ off the ground. See the Toilevator Toilet Riser, 500 lb Capacity Most Popular Raised Toilet Seat Hinged Elevated Toilet Seat – 3″ – Perfect for the men in the house, this device raises the seat by 3 inches but also allows the ring to be lifted the same as your standard toilet seat.

It barely changes the look of the toilet. Use the following “Raised Toilet Seat Buyer’s Guide” to help decide which toilet seat is right for you or your loved one.
Puppy Age Sale Laws Raised Toilet Seat Buyer’s Guide
Remove Kitchen Faucet Youtube Short Term Use – Non-locking Raised Toilet Seats – For short recovery times, occasional use or some post-surgery, the raised toilet seats without locking devices work fine.
Jeep Cherokee Seat Covers CheapThey are portable and very easy to use. Depending on the stability of the user, we recommend that these be used along with a Toilet Safety Frame since these elevated toilet seats are attached by reliable methods, but not clamped or bolted on for increased security.

Medium Term Use – Locking device – Special locking devices, front-clamps and brackets keep these raised toilet seats from shifting providing a secure, comfortable toileting experience. A fantastic alternative to permanent fixation. Long Term Use – Bolt on Toilet Seat – Perfect for disabled, elderly or those with a chronic need for an elevated toilet seat. These raised toilet seats are super secure and have many helpful features to make getting on and off the toilet much easier. Hip Replacements, Post Surgery, Leg, Hip and Knee Injuries and Fractures often require a unique, asymmetrical shaped toilet seat riser with one side “cut out” to allow one leg to remain in the prescribed position while sitting (knee should be lower than the new hip during hip replacement recovery). Bariatric, Heavy Duty, Extra Wide Raised Toilet Seats– Choose from styles that accomodate users up to 600 lbs. Wheelchair Transfer Toilet Seats – Convert your toilet into an elevated wheelchair transfer seat.

Bolts onto most standard toilets. Please call an Allegro Customer Care agent at 800-861-3211 if you require further assistance in choosing the right raised toilet seat or see all Raised Toilet Seats for more ideas. Pudendal nerve entrapment (PNE), also known as Alcock canal syndrome,[1][2] is an uncommon[1][3][4][5] source of chronic pain, in which the pudendal nerve (located in the pelvis) is entrapped or compressed.[6] Pain is positional and is worsened by sitting. Other symptoms include genital numbness, fecal incontinence and urinary incontinence. The term pudendal neuralgia (PN) is used interchangeably with "pudendal nerve entrapment", but a 2009 review study found both that "prevalence of PN is unknown and it seems to be a rare event" and that "there is no evidence to support equating the presence of this syndrome with a diagnosis of pudendal nerve entrapment," meaning that it is possible to have all the symptoms of pudendal nerve entrapment (otherwise known as pudendal neuralgia) based on the criteria specified at Nantes

in 2006, without having an entrapped pudendal nerve. A 2015 study of 13 normal female cadavers found that the pudendal nerve was attached or fixed to the sacrospinous ligament in all cadavers studied, suggesting that the diagnosis of pudendal nerve entrapment may be overestimated. There are no specific clinical signs or complementary test results for this condition.[9] The typical symptoms of PNE or PN are seen, for example, in male competitive cyclists (it is often called "cyclist syndrome"[5]), who can rarely develop recurrent numbness of the penis and scrotum after prolonged cycling, or an altered sensation of ejaculation, with disturbance of micturition (urination) and reduced awareness of defecation.[11] Nerve entrapment syndromes, presenting as genitalia numbness, are amongst the most common bicycling associated urogenital problems. The pain is typically caused by sitting, relieved by standing, and is absent when recumbent (lying down) or sitting on a toilet seat.[13] If the perineal pain is positional (changes with the patient's position, for example sitting or standing), this suggests a tunnel syndrome.

[14] Anesthesiologist John S. McDonald of UCLA reports that sitting pain relieved by standing or sitting on a toilet seat is the most reliable diagnostic parameter. Other than positional pain and numbness, the main symptoms are fecal incontinence and urinary incontinence. Differential diagnosis should consider the far commoner conditions chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis. Similar to a tinel sign digital palpitation of the ischial spine may produce pain. In contrast, patients may report temporary relief with a diagnostic pudendal nerve block (see Injections), typically infiltrated near the ischial spine. Electromyography can be used to measure motor latency along the pudendal nerve. A greater than normal conduction delay can indicate entrapment of the nerve. Imaging studies using MR neurography may be useful. In patients with unilateral pudendal entrapment in the Alcock's canal, it is typical to see asymmetric swelling and hyperintensity affecting the pudendal neurovascular bundle.
PNE can be caused by pregnancy, scarring due to surgery, accidents and surgical mishaps.[19] Anatomic abnormalities can result in PNE due to the pudendal nerve being fused to different parts of the anatomy, or trapped between the sacrotuberous and sacrospinalis ligaments. Heavy and prolonged bicycling, especially if an inappropriately shaped or incorrectly positioned bicycle seat is used, may eventually thicken the sacrotuberous and/or sacrospinous ligaments and trap the nerve between them, resulting in PNE. Optional treatments include behavioral modifications, physical therapy, analgesics and other medications, pudendal nerve block, and surgical nerve decompression.[7] A newer form of treatment is pulsed radiofrequency. There are stretches and exercises which have provided reduced levels of pain for some people. There are different sources of pain for people since there are so many ligament, muscles and nerves in the area. Sometimes women do pelvic floor exercises for compression after childbirth.

However, there have been cases where the wrong stretches make the constant pain worse. Some people need to strengthen the muscles, others should stretch, while for some people it is purely neurological. There have been cases where doing stretches have helped bicyclists. Acupuncture has helped decrease pain levels for some people, but is generally ineffective.[] Chiropractic adjustments to the lower back have also helped some patients with pudendal nerve issues. There are numerous pharmaceutical treatments for neuropathic pain associated with pudendal neuralgia. Drugs used include anti-epileptics (like gabapentin[20]), antidepressants (like amitriptyline[13]), and palmitoylethanolamide. Alcock canal infiltration with corticosteroids is a minimally invasive technique which allows for pain relief and could be tried when physical therapy has failed and before surgery. A long-acting local anesthetic (bupivacaine hydrochloride) and a corticosteroid (e.g. methylprednisolone) are injected to provide immediate pudendal anesthesia.

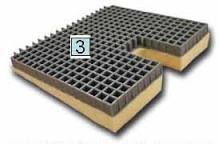
[13] The injections may also bring a long-term response because the anti-inflammatory effects of the steroid and steroid-induced fat necrosis can reduce inflammation in the region around the nerve and decrease pressure on the nerve itself. This treatment may be effective in 65–73% of patients. Pulsed radiofrequency has been successful in treating a refractory case of PNE. Various ergonomic devices can be used to allow an individual to sit while helping to take pressure off of the nerve. With bicycles the seat height and tilt can be adjusted to help alleviate compression. There are also bicycle seats designed to prevent pudendal nerve compression, these seats usually have a narrow channel in the middle of them. For sitting on hard surfaces, a cushion or coccyx cushion can be used to take pressure off the nerves. Decompression surgery is a "last resort", according to surgeons who perform the operation.[14] The surgery is performed by a small number of surgeons in a limited number of countries.

The validity of decompression surgery as a treatment and the existence of entrapment as a cause of pelvic pain are highly controversial.[23] While a few doctors will prescribe decompression surgery, most will not. Notably, in February 2003 the European Association of Urology in its Guidelines on Pelvic Pain said[24] that expert centers in Europe have found no cases of PNE and that surgical success is rare: Pudendal nerve neuropathy is likely to be a probable diagnosis if the pain is unilateral, has a burning quality and is exacerbated by unilateral rectal palpation of the ischial spine, with delayed pudendal motor latency on that side only. However, such cases account for only a small proportion of all those presenting with perineal pain. Proof of diagnosis rests on pain relief following decompression of the nerve in Alcock’s canal and is rarely achieved. The value of the clinical neurophysiological investigations is debatable; some centres in Europe claim that the investigations have great sensitivity, while other centres, which also have a specialized interest in pelvic floor neurophysiology, have not identified any cases.